
In a first for Jerusalem, doctors at Hadassah Hebrew University Medical Center in Ein Kerem recently performed an Endoscopic Sleeve Gastroplasty (ESG) procedure.
The ESG procedure “can result in significant weight loss, but with a faster recovery times, fewer side effects and lower rate of complication as compared to bariatric surgical procedures,” Hadassah said in a statement.

“Some patients, such as those with advanced liver disease, are at high risk for procedure, and ESG is their best option for weight loss,” Dr. Ariel Benson of the Institute of Gastroenterology and Hepatology’s Advanced Endoscopy Unit at Hadassah told The Jerusalem Post on Tuesday.
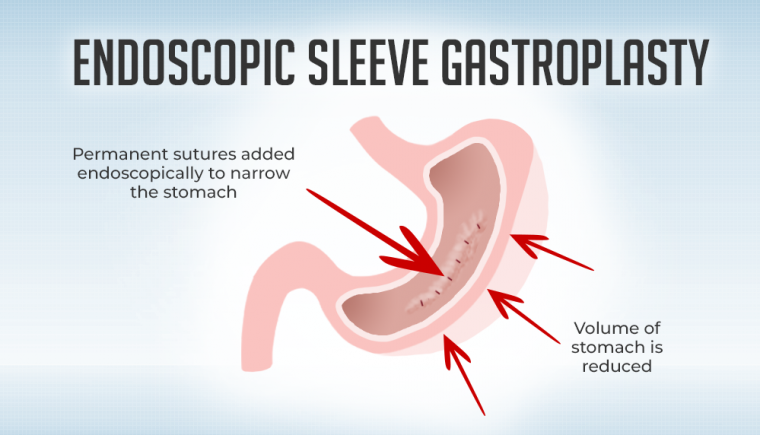
ESG “is a relatively new type of weight-loss procedure that is minimally invasive and makes the size of the stomach smaller, thereby minimizing the intake of food,” he said. “It is performed via endoscopy, advancing a small camera through the mouth and into the stomach, without any external cuts on your body. Then, through the endoscope or flexible camera, we place internal stitches in the stomach, which reshapes and reduces the size of the stomach, resulting in weight loss.”
The procedure, which lasts one to two hours, is performed under general anesthetic.
Benson said people with overweight background diseases who do not meet these criteria do not receive permission to undergo bariatric procedure, “even though their excess weight is one of the major causes of the illnesses they suffer from.”
The hospital first began the procedure with an endoscopic abdominal shortening procedure, which is for people who are not fit for bariatric procedure, “but need it very much medically, or for patients who are not interested in classic and familiar surgical bariatric procedure,” he said.
ESG allows for an additional weight-loss option for patients who suffer from obesity, Benson said, and, in some cases, “It is the only weight loss procedure for those who are at too high a risk for procedure.”
“ESG is a great choice for these patients, as the risks of ESG are lower than that of procedure while at the same time resulting in weight loss,” he said. “Since the weight loss seen with ESG may be less than procedure, the benefits of ESG are the lower risks and that it is minimally invasive.”
Some patients who do not meet criteria for bariatric procedure can benefit from ESG, including patients with diabetes who require weight loss as part of their treatment regimen but do not have a high enough BMI to qualify for procedure, Benson said.
“ESG is also an option for all patients who are looking for nonsurgical ways to lose weight,” he said. “Only a small percentage of obese patients receive treatment with bariatric procedure, since many patients are hesitant to undergo procedure with the risks involved.”
Many people are unable to achieve effective weight loss with lifestyle changes and diet, and ESG is a nonsurgical weight-loss treatment that can help fill the treatment gap, Benson said.
The medical center said this technique is used to treat overweight people who do not fulfill “the classic and familiar criterion to receive bariatric procedure.”
The procedure was performed by a team of experts from Hadassah together with Dr. Michel Kahaleh from New Jersey, one of the pioneers of the endoscopic method, who came specifically to perform the procedure at the hospital.
A 48-year-old Jerusalem resident identified as D, who was the first to receive the ESG procedure at Hadassah, said: “About 20 years ago I started gaining weight. It bothered me, but at first not too much.”
“I tried different diets, managed for a period, and each time I broke down,” he said. “I reached 110 kg. It’s not really fat, but there were health problems that I developed from the excess weight.”
Following this, D was diagnosed 10 years ago with diabetes and then high blood pressure and too many triglycerides, which is a type of fat, in the blood.
“I was given medication, and it was static until about a year ago I had severe liver problems,” he said.
The problems worsened over time until he developed cirrhosis of the liver, which can destroy the organ.
“The doctors who treated me told me that the excess weight I suffer from is the foundation for all my ailments and that I must lose weight, but this was not an option in my position,” he said.
D decided to do gastric bypass “because I couldn’t lose weight in any way. I started going through the process of bariatric gastric shortening. But a test that measures the body’s BMI determined that I was not fit enough for the surgery.”

“Although it was close, I was told I won’t get permission to go through the surgery I so badly wanted,” D said. “I was very frustrated, but luckily… I was treated at Hadassah, and my doctors – Dr. David Hakimian, an internal-medicine specialist, and Dr. Ram Elazary, the director of the Hadassah Bariatric Unit – thought outside the box and offered me a new type of abdominal procedure that fits people exactly in my condition.”
Hakimian said D came in with a high grade of cirrhosis caused by obesity and various medications he had taken over the years due to various diseases.
“It was clear to all of us that needed to lose weight” and needed “an aggressive treatment that could improve liver disease and life,” and this is what led to the decision to perform the ESG procedure, he said.
Several days after the operation, D had already returned to work, and now, a few weeks later, he has already lost eight kg.
Dr. Harold Jacob, a senior physician at the hospital’s Institute of Gastroenterology and Liver Disease and director of the Endoscopic Unit, said ESG procedure “is a surgical breakthrough” for patients in this position.