 The bacteriophage (depicted here) is a bacterium’s worst nightmare.
The bacteriophage (depicted here) is a bacterium’s worst nightmare.
A hospital in Israel used bacteriophages and antibiotics to successfully treat a multidrug-resistant left tibial infection in a man who was injured in an auto accident, saving his leg from amputation, researchers said.
The bone was infected with two bacterial species — extensively drug-resistant (XDR) Acinetobacter baumannii and multidrug-resistant (MDR) Klebsiella pneumoniae, according to findings published in Clinical Infectious Diseases. After treating the infection, researchers noted that they were able to develop a phage-resistant A. baumannii mutant in vitro, and then isolate a new phage to combat it, “ the potential flexibility of phage treatments.”
Ran Nir-Paz, MD , infectious disease specialist at Hadassah-Hebrew Medical Center, and Ronen Hazan, head of the phage therapy lab at Hebrew University, said the case contributes to the expanding knowledge of phage therapy in several ways.
“First, we succeeded to treat an infection with two bacteria in which we could show in the lab that they probably protect each other from the antibiotics. Second, we showed by simulation in the lab that if a resistant mutant would emerge, we would be able to treat it. Third, this work is a rare example of voluntary collaboration between clinicians,” they told Infectious Disease News.
“This was the first treatment in Israel, which we hope will lead to the establishment of an advance center of personal, adaptive and dynamic research and treatments of infectious diseases medicine.”
The study focused on a 42-year-old man admitted to the trauma unit of Hadassah-Hebrew University Medical Center after a motor vehicle accident with a left bicondylar tibial plateau fracture with compartment syndrome and a right distal femoral fracture, the authors explained.
Six weeks after admission, physicians discovered the left tibia infection with XDR A. baumannii and MDR K. pneumoniae. According to the study, the wound was treated with serial irrigation, debridement, the placement of a cement spacer due to bone loss, and 6 weeks of piperacillin/tazobactam, followed by an 8-week course of meropenem and high-dose colistin, all of which failed to clear the infection.
After the patient refused an above-the-knee amputation 7 months into his hospital stay, doctors turned to a combination of bacteriophage therapy targeting the two bacterial strains, plus IV meropenem and colistin.
Within days, there were signs of wound recovery, graft healing and elimination of subtle chronic bone pain in the patient’s leg, the authors reported. During an 8-month post-treatment follow-up, no positive cultures for either A. baumannii or K. pneumoniae were found. The wound closed, the patient’s pain subsided and blood, stool, urine and saliva samples were all clear of bacterial isolates, they reported.
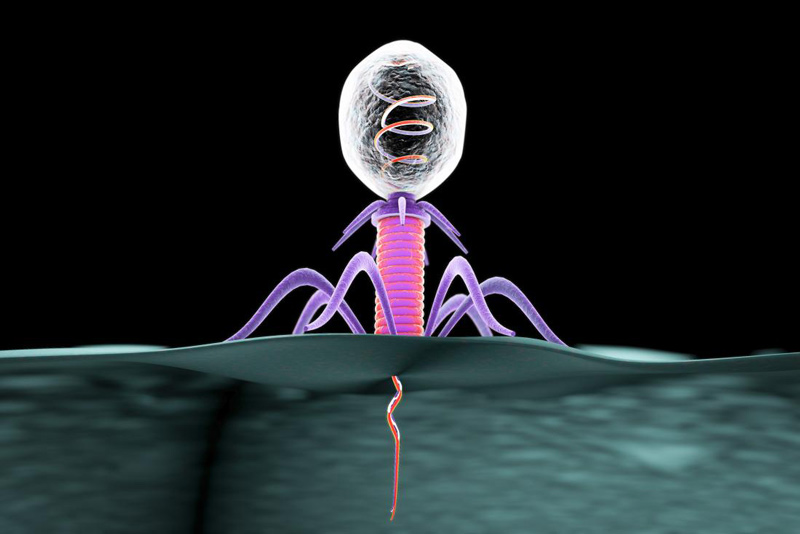 Bacteriophages (depicted here) may provide an insight into bacterial infections.
Bacteriophages (depicted here) may provide an insight into bacterial infections.